The more I get into the research on antidepressants, the more questions I have. In the last post, I raised issues about the endless search for the right medication; the discouraging record of relapse after becoming symptom-free; and the puzzling primacy of antidepressant treatment for an illness with complex causes that go way beyond biology.
Those questions are only the starters. I have even greater concern about long-term antidepressant treatment. Most psychiatrists consider it necessary for severe, recurrent illness, but others – apparently a small minority – are speaking out about adverse effects of using these drugs for prolonged periods.
My experience with long-term treatment has made me skeptical of the value of antidepressants, but recent studies make me worry that I might have been harmed as well. So I’m looking for an answer to a question that I’d rather not have to ask at all.
Can long-term antidepressant use worsen depression?
Many Antidepressants, Little Relief
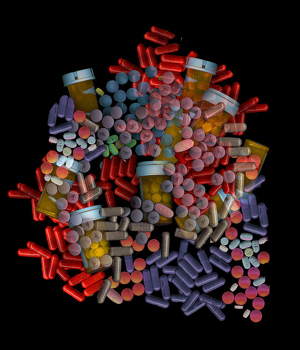
For years, I was convinced of the necessity of taking these drugs. I had no hesitation about taking multiple meds for depression, anxiety, poor concentration and sleep problems – 20 different drugs over the last 16 years.
Over time, it became clear that antidepressants weren’t doing much for me. Nevertheless, I kept thinking that I’d be in worse shape if I stopped. In other words, I was driven by fear. So I kept on going and wound up taking at least one sample of each class of antidepressants:
- Selective Serotonin Reuptake Inhibitors (RI) (Zoloft, Paxil, Celexa, Lexapro, Luvox)
- Serotonin Norepinephine RI (Effexor, Cymbalta)
- Norepinephrine Dopamine RI (Wellbutrin)
- Norepinephrine RI (Strattera)
- Tricyclic (Imipramine)
- Atypical (Trazodone)
I took some of these alone but more often in combinations. I also used other drugs to help with mental energy and concentration, anxiety and insomnia.
The guiding assumption of all the psychiatrists who treated me was that failure of one medication should be followed by others until an effective one was found. No psychiatrist ever suggested that I should stop using antidepressants. They assumed that stopping treatment would lead to relapse. (It didn’t seem to matter that I had not recovered enough to qualify for relapse.)
Depression gets worse, then better – for a while.
During this long period, the recurring major depressive episodes became more and more severe, but that wasn’t the worst of it. Episodes come and go, but I also noticed a gradual deterioration of short-term memory and the ability to concentrate. Anxiety in groups skyrocketed, and I also had frequent periods of feeling dissociated from everything around me. These were the problems that eventually made it impossible to my professional work.
However, I did improve a great deal with my 12th antidepressant. This was an MAOI (monoamine oxidase inhibitor), a class of antidepressants regarded now as a last resort because it requires dietary restrictions. Twelve years of misery with major depression is a poor tradeoff for a few items in my diet, but that’s the way it worked out.
The MAOI I’m using is Emsam, or selegiline taken through a 24-hour patch. This wasn’t the final word, however. It failed after a great year and a half and was then supplemented with lamotrigine, a mood stabilizer used to treat bipolar illness. (Before lamotrigine, I tried lithium, another mood stabilizer, but that made me feel as if all my brain circuits had been disconnected.)
The addition of lamotrigine to Emsam restored me again, this time for about two years. I intend to withdraw from these drugs over a very long period of time since they don’t seem to be doing much now. But there won’t be any more medications after this. I’ve found other types of treatment to keep myself healthy.
What was the effect of all these drugs?
The accepted wisdom is that I should stay with antidepressants because there’s a strong likelihood that I’ll head into another major depressive episode soon after I stop. I have to say that my highly unscientific reaction to that idea is – No-duh.
After all, my brain’s neurotransmitter systems have been getting used to living on various drugs for 16 years. They must have made some adaptation by now to this steady, artificial diet. So, sure, there will be a reaction after you stop pumping drugs in there.
Is there any evidence that the brain really does adapt in this way?
That question leads to a much greater concern. Why have the symptoms of depression progressively worsened over time, despite constant medication? Is it possible that the drugs designed to prevent relapse have done more long-term harm than good? Would I have been better off if I had never taken antidepressants at all?
Of course, I’ll never know for sure what might have been, but I have found studies that answer “maybe” to these disturbing questions.
Can long-term antidepressant treatment cause harm?
Giovanni Fava has been posing the question of potential long-term changes in brain function caused by antidepressants since the early 1990’s. In a 2010 paper, he says that antidepressants are crucial for the treatment of depressive episodes in the acute phase when untreated symptoms are at their worst. With long-term use, however, the brain sets to work compensating for the drug-induced changes with a process he calls oppositional tolerance.
The brain tries to re-establish its usual balance of production, release and reuptake of neurotransmitters – as every system of the body does when its normal functioning has been disturbed. The idea is that if the medication artificially jacks up the brain’s level of serotonin or norepinephrine, the neurobiology of the system reacts by reducing its own production of the neurotransmitter. In other words, if antidepressant use continues long enough, the brain will create a system to cancel out its effect.
A paper published this year adds to Fava’s findings the new idea of tardive dysphoria, a slow-onset depression induced by long-term medication use. The lead researcher, Rif El Mallakh, points out that resistance to treatment with antidepressants has dramatically increased, from 10-15% of patients in the early 90s to 40% in 2006. This corresponds to the period of explosive growth in the use of these drugs, especially for long-term maintenance treatment designed to protect against relapse.
There are many possible reasons for this huge change, but he focuses on the possibility that antidepressant use itself could be causing the problem. He discusses specific neurobiological reactions that could account for the emergence of higher levels of resistance to treatment. In addition, he cites evidence that stopping antidepressants in people who no longer respond to them can lead to reversal of symptoms as the brain compensates once more, this time for the withdrawal of the drugs. For some people, however, stopping the medication has no effect. They continue to have recurring depression. If antidepressant treatment is restored as a response, these patients can develop a permanently recurring illness. This is tardive dysphoria.
Could this explain my history with antidepressants? It’s a little late to freak out, but … !
Mainstream practice: stay with antidepressants
The general attitude among psychiatrists is firmly on the side of long-term, even lifetime, use of antidepressants as the best protection against relapse. This is the recommended treatment for people with my condition – numerous recurrences of depression over many years, high frequency of recurrence and a family history of the illness. The rationale for this approach is that patients on extended drug use have less chance of relapse than those who go untreated.
I have trouble following the evidence and reasoning that leads to this treatment recommendation, but I’ll save that for another post.
You can read an interesting report on a roundtable discussion among 6 psychiatrists who strongly believe in long-term treatment with antidepressants. Their views are not monolithic and reveal a lot of debate within this community of practitioners. The paper is Preventing Recurrent Depression: Long-Term Treatment for Major Depressive Disorder.
I’d like to think that my experience with antidepressants, while it may have been pretty disappointing, didn’t worsen my condition. But now I’m finding that these drugs could have done a lot more harm than good.
I can’t change the past, but I hope my history with medications isn’t going to cloud my future.
Robert Whitaker has explored all these questions about treatment for depression and other mental illnesses in Anatomy of an Epidemic. He also has a good article on tardive dysphoria on his blog at Psychology Today.
Image by psyberartist at Flickr


I’ve been on Celexea for over 25 years and have tried twice to get off the meds. The realization that My brain is now dependent on them scares the heck out of me, but ever time I try I get light headed, fainting spells, lack of concentration more so than normal and on and on. What to do ?
I have started to believe that it’s ok to be on antidepressants for a short period of time Hilary Davies as I believe they can stabilise a persons mood, in which I then think is the perfect time to have cbt therapy and psychotherapy also! I honestly don’t think that being on medication long term does anyone any favours! Although this is only from my own experience! I have noticed that Dr’s literally put ppl on tablets bcoz there are no services to support the amount of people with mental health problems and so gp’s literally give meds out easily as they are not specifically experts in mental health, they really do not have any other options and definitely do not have time or funding for any other options! For so many yrs government has refused to accept that mental health was an illness and so any services or funding were axed as not seen as important! Which is why we have a crisis in this area! Xx
I have spent some time reading the comments and it almost brings tears to my eyes…except I can’t cry and you will find out why that is, right away. First of all I really hope this gets printed because what happened to me will blow your mind more than any AD on earth.
I lost a mom at 9 years old and I don’t care who you are…it will blow a hole through your life faster than anything…she had dealt with depression. Growing up its very clear my dad never helped her situation much and quite possibly contributed to it. My mom protected me from beatings my dad would occasionally give….no protection when she was gone though.
Growing up my dad threatened me with 2×4”s to the head and the last straw was when at 17 my dad tried to break my neck unprovoked….nice. I moved out and just before I moved out I started dealing with a depression from hell and it turned out to be bipolar 2 for the most part. I live on Canada and our Dr’s here are subpar as it gets, there’s a few good ones but overall it’s a joke at best.
I’m trying to get to my point here so bear with me. My life was basically a rhino”s arse for many years taking one garbage med after another (they’re all garbage…trust me I’ve studied this thoroughly) prescribed by a Dr that was such a pathetic fool he would give put meds like candy at Halloween and even admitted he was terrible at combining meds…so his main tool to treat depression was useless in his hands. I stopped sering him when I ran into another Dr on a repeat hospital stay. My fiends mom thought the Dr was a certified quack…he wasn’t alone in that category.
This new Dr was better at putting meds together but had zero psychotherapy skills…less than zero. In fact, he would make fun of you if you mentioned what was on your mind…what a sweetheart. There was only one problem with this Dr…once on a med you were on it for life! Even if it didn’t work you were stuck on it, this later ruined my life. Around the mid 2000”s I started to get a grip of things and landed a good job after doing construction jobs that were a waste of my interpersonal skills and started working for a very large company (huge) and with my enthusiasm and ability to work my butt off I started making good money and became highly respected. A couple of years I met this girl online and had no idea the person was a control freak and had serious anger issues among other things. After two months I had seen enough bs to realize this person was not a very empathetic person…at all and I ended up moving in.
This person and my Dr, pharmacy ended up ruining my life. There was some serious red flags after we started dating and I had more than enough reason to get the heck out if the relationship but I didn’t and I’m a moron for that. She was professional at giving the silent treatment, was skilled at laying guilt and it was her way or the highway (what a beautiful person)
I started getting depressed not long after and I should’ve got the hell out of there. I was for the most part depression free for a number of years and now I was heading into a depression something fierce. This was time to get out of the relationship but I was a moron and let my retarded head take over. I started taking natural supplements instead of reaching for pills right away and they didn’t do too much…the health food store never recommended the right ones.
After a few months of hanging in a coworker gave some valium since I mentioned I was dealing with depression and anxiety. He was not the most stable person on earth and he should’ve NEVER offered me his drugs….NEVER!!! I took half of one the next day and got a massive headache, should’ve brought the remaining ones back and said thanks but no thanks. Being an idiot, I left them on my dresser and on Xmas day I had the full blown idiotic idea to try another one before going to my partners family gathering (family was humoungous).
This time I didn’t get a headache and it took care of the anxiety nicely. Next month asked for valium and my Dr said no! It’s addictive! (Remember this). Caught off guard, I then said what about taking lamictal/gabapentin since it kind of worked a number of years ago. He said okay but before I was taking the name brand and now it was generic..
I had no idea the generic was basically suicidal thoughts in a bottle….I’m being nice since big pharma and the fda are the best lovers on earth and corruption is at the Mad comic book level!
After brig on the generic lami for a month and a bit I went straight into the outhouse as far as moods go….I should’ve got off this junk but my Dr would just keep prescribing away. At the two month mark my anxiety and depression were easily 5x worse before meds. I then mentioned that a coworker gave some valium and it mad me calm, right away my Dr says “I’ll give you valium!” and I received a bottle of hundreds of valium…I guess it wasn’t addicting anymore!
Here’s where my life gets ruined (oh, it’s done make no mistake). My Dr kept me in the garbage lamictal for a whole year along with the valium and at the end of that year I got so sick I had to take time off from work, AND MY DR STILL KEPT ME ON THE SAME MEDS!!! A blind man would see a problem with this! After getting better on my own taking natural supplements I told my Dr he can forget about the dangerous lamictal! It did lots for me, let’s see…hair loss, lowered immune function, gray hair, dry skin, insomnia and I almost lost my eye site (binds with melanin…don’t take this junk).
What I didn’t know was the gaba/lami had a ferocious withdrawal that was out of this world. I ended up going back on it briefly (no wonder GSK was fined 3 BILLION dollars for lying about clinical results and witholding negative outcomes ,you still want to take meds now?!)
After two years of this complete mockery of a Dr I was still on valium for 2 YEARS!!!! 2 YEARS!!!! Hey, if it’s addictive might as well have a patient stay on it till they are good and dependent on it…yes sir. I then mentioned to my Dr that I was still depressed and he said “Valium can cause depression…you know? No, I didn’t know and what he should’ve known was you shouldn’t give valium to a person that has depression…it says it online so it surely must be common knowledge amongst professional…or non-professionals for that matter.
I thought right then he would take me off but nope…keep on taking it. After a few more months of this bs I started getting ringing in my ears and went on a crappy website that said valium can cause it…they forgot to mention ALL benzos can cause it…ALL of them. I made a mistake of not telling anyone I was going off it including my Dr because he would never take me off it on his own never. Three weeks after a one month taper I started getting withdrawals and they caught me off guard….seriously three weeks later?!
I went to see my Dr and told him my anxiety was through the roof and I needed something for anxiety (I was only on value at this point) and he never even asked about the valium, I didn’t realize they were withdrawals. He then put me on alprazolam…you CAN’T go on alprazolam after valium…won’t find anything on Google representing that. In fact, you’ll just get results going from alprazolam to valium…Dr was a fool!
The alprazolam made me feel like crap instantly and I was getting massive interspersed withdrawals after just three hours and my Dr only gave me two a day to take. If he used his brain, he would’ve asked about the valium and I would’ve been back onto a slower taper from valium.
I took time off work again and this was completely unnecessary to say the least and two weeks later my Dr prescribed a combo of doxepin(one of THE most dangerous AD on earth and combined it with 300 mg of lithium. I didn’t freaking need this! He never even asked my opinion on this bs and just phones in the dangerous meds! I was feeling okay that morning but his senile receptionist refused to let me in at my appointment and at that time I was hitting the bad withdrawals from the alprazolam. The Dr just took over like an idiot and didn’t listen to me one bit (I found out he was going through financial problems and couldn’t afford his taxes..
He shouldn’t have been practicing psychiatry at this point).
When I told him I was feeling rough, right away he looked at my chart and said” I don’t have you on an antidepressant” he should’ve done the same thing a month earlier when I said I needed something for anxiety!? I told him I didn’t want a AD I was taking natural supplements. He completely ignored that and then asked if I ever had doxepin and I said I never heard of it. He then asked how my sleep was and I said it was good around 7 hours of sleep.
He ignores that too and said it’s good for sleep. He then picked up the phone and called in a prescription adding lithium of all things!!!. After he gets off the phone I was sitting there kind of shocked about what transpired…I just came in to touch base and now was walking away with a med I never heard of or didn’t want. Before I left I asked my Dr if it was safe to take theseeds with my natural supplements and he said “absolutely!” I then mentioned I ordered another supplement online and I was going to receive it next month and told him the name. He even wrote it down and said “no problem”.
I was sh*t scared of this combo for some reason and after reading the reviews about doxepin several people said it ruined their lives. I dealt with Safeway pharmacy and the mgr admitted they never checked for interactions…at all (this was after the fact) and whenjoy I called the pharmacy and asked if the meds were safe, a woman that could BARELY speak English said “yes, it’s safe. What time are you going to pick it up?” This pharmacy was run by a jerk mgr and on top of that they would put pressure in you to pick up meds that day…or they would get very angry. I should told the pharmacist you can keep the meds and I’m going to take my business elsewhere( this would’ve saved my life) but I was concerned about my insurance company on the Dr’s forms asking if the paitient was taking medication as prescribed so I thought I better pick it up. Manulife is unethical.
I then went to get it with zero warning of a potential interaction…NOTHING. I wasn’t even asked if I took them before or had any questions. I went home very concerned about these meds. Finally around 10pm I thought I’d give them a try, I was feeling very sick because I was going through extreme withdrawals from the two a day alprazolam.
I woke up in the middle of the night with the most horrific nightmare of my life, doxepin gives you nightmares that will make the scariest movie look like a walk in the park. The other thing it does is it makes getting up like waking from death. My fiance and u were going on a trip that day but I had no idea when and my fiance got violently angry when I couldn’t get out if bed when she asked and started screaming at me to clean the house because we were having a house sitter. I dragged my ass out of bed and I mean DRAGGED and got the house looking great, showered and shaved and packed in time to go.
The only problem was, my fiance took on too much work before we left and she took it out on…you guessed it…me, and I was so screwed up from the doxepin that I couldn’t keep my eyes open. We drove for six hours and not only did I get complete silent treatment, she was getting very angry and I should’ve got the hell out of the car right when she slammed the trunk like she tried to break it off.
Six solid hours of silent treatment when I could barely keep my eyes open. My fiance was a real prize. Upon getting to the first destination she wanted to go for a walk…she then said she wanted to break up with me. That’s the equivalent of a corrupt politician asking for the public’s trust after ripping them off. I was shocked and screwed up…you give me six hours of unnecessary silent treatment because of your own problems (silent treatment is considered the most severe form of non physical abuse)and you want to break up with ME???
Why did she just let me stay home and not have to deal with her filth. Well, she then said we don’t have to break up after all. What a complete her, if I wasn’t so sick I would’ve said “yes we do, and I would’ve gone home”. I took my pills that night and the next day I felt very sick, we drove all day and we got to a bnb at 10 pm. She went on the laptop and I pulled out my meds, I had the meds in my hand and said put loud “I don’t want to take these, they’re making me sick.”
“NO, YOU HAVE TO GIVE THEM TWO WEEKS!” My fiance screamed. I was shocked, hey when you are feeling sick from pills YOU STOP THEM! Right away I thought that if I dont take them I was going to get more angry silent treatment. I then told her to look up on the Internet how ganger pus these drugs were before she demanded I keep taking them. No, I’m not going to look them up she said.
Two weeks later I was rushed to hospital with brain damage, muscle damage, severe nervous system damage and kidney damage. The hospital never took it seriously and screamed at me and left me in a wheelchair to die (I live in Canada and our health care system is one of the worst on earth…don’t believe what you hear…it’s that bad)
A Dr casually walked up to me 5 hours after getting there and said I could go home it’s a panic attack…I tried to tell them it wasn’t a panic attack but a reaction. But they just said you can go home. I went home and woke up with all the damage and urinating blood.
Alright, cool. The hospital tried to cover up the fact they didn’t triage me, with a fake triage report. ..I already had a copy of the original. My Dr changed his notes completely and had a private conversation with the pharmacist to devise a plan and my fiance was absolutely zero help and nit even on my side regarding the damage and negligence.
Yeah, I’m a bit mad. That’s an understatement, I uncovered cover ups, by everyone involved and there’s even a question of wondering if taking meds is good for your depression?! Absolutely not! The pharmaceutical company NEVER returned my calls, the health “professionals”
Did cover up after cover up and people here want to know if meds can work or not. Of course not, it’s a complete scam…look up the lawsuits against these big pharma companies and the record setting fines! They do their own clinical testing behind closed doors and only have to provide two positive outcomes. How do we know they didn’t fudge the numbers? How do we know that people didn’t get worse? How do we know what happens after 6 months?
Big pharma meds are ONLY tested for 6 months….after that YOU are a guinea pig. Biggest scam in the history of medicine and they know this. Why is it these meds get approved and as soon as the patent runs out they are pulled off the market?! Foes anybody remember Vioxx? That killed 60,000 people! 60,000!!!! Someone should’ve received the death penalty never mind a fine!!!
Think about that. 60,000 people died from that drug, how many people have died during 9/11? And they went out and dropped bombs like crazy and lots of fine service people perished on top of that. I’m making a crude comparison but someone has to, big pharmacy is a complete utter joke and these meds cause more problems than they help and that’s a proven fact.
Name one thing psychiatry has cured, I won’t hold my breath for the answer because I would die. Psychiatry is medicines dirty secret and we are getting conned and scammed with these dangerous meds that I guarantee you the ceo of these companies would never let their kids take these monstrosities.
Sorry for the long post but my life is ruined, it’s gone, there’s nothing left for me anymore. I can barely work, I barely sleep and since this reaction happened I have thought of dying many thousands of times. You would too if you were as screwed up as I am, I’m barely existing now because of a stupid, pathetic Dr, a terrible pharmacy, a stupid corrupt hospital and a fiance that was an integral part of my damage when she demanded I keep taking the dangerous meds.
Ruined my life and I mean it ruined my life. Dr’s, nurses are all corrupt as well…when’s the last time a Dr went to jail for killing someone over negligence? Not too often I tell you but I seriously think the death penalty should be brought in for Dr’s and big pharma.
Thanks for reading.
So sorry Rod , To hear your story, so sad , all of it , and your right about it all !! I went through 9 yrs.’ of their med game , and never needed nor should have been on any of it , I fought for my life , thinking the drs knew what they were doing , how could they be so stupid or were they really just trying to kill me I ask myself now , after just watching the hospital kill my best friend and I kept telling them if they didn’t stop giving him the same meds that were given to me what was going to happen !! and they would kill him and they did. I was very healthy started working out at 21, was really in to it , addicted, ate well took vits ect, took very good care of myself , then I started noticing I seemed to be having a lot of constipation so I dealt with it and then one day I was talking to someone that said I could have IBS so I decided to go to dr , boy worse mistake of my life , They tried convincing me I had anxiety and depression , wanting to give me meds , I said no , went home , months later went back, about the constipation, and then my night mare began , while the drs own words , were flipping coins to figure out what was wrong with me , I am fighting for my life , being ambulanced in and out of hospitals for 9 yrs , then ended up with holes in my heart from the meds and fighting pain all those yrs , What really made me sick was when they acted so shock when they asked me at 48 yrs old my age , and how many kids have I had as they kept looking at my chart and back at me like I lying to them , and then comes back with DO YOU REALISE YOU HAVE THE INSIDES OF A 20 YR OLD , I thought yea but I bet I wont by the time you get through with me , they ruined my life , there’s more to the story , just to much to write , and I also had a piece of crap as a mate that only made things worse ,was a really tough fight and am still dealing with health issues bcos of it now , so sorry about your Mama and all you went thru.
Wow! That’s quite an experience you had. I also live in Canada and putting yourself in the hands of Canadian doctors is like throwing yourself in front of a train. I took different meds of the antidepressant type and sometimes was prescribed an antipsychotic along with them. I’m not psychotic, but Drs are told that the efficacy of ADs are greater along with an antipsychotic. Now I have to still take the AD at a quarter of my last dose, which was half of what I was on before. My family wants me totally off of it, because it changes my personality so much and not in a good way. I used to have an excellent memory and now it’s horrible. I’ve done things I later have know recollection of whatsoever. Probably only a bit gets back to me. I’ve had to go on disability, because I’m unable to function anymore. I wish I had just endured my normal course of depression, which always resolves within two years time.
I wrote to the psychiatrist about the things I experienced, asking his opinion. It’s been months and he never got back to me. It’s like they ruin your life and when they are satisfied they move on to the next victim, leaving a path of carnage along the way.
Hi everyone, thanks for your insightful responses, until medicine is non-for – profit and there are serious regulations on what doctors can prescribe, the consumer loses. I’ve been on pills from the tender age of 12 (I’m 44 now). I tried to stick to my regimen, but it’s always derailed by insurance, health issues, serious side effects and withdrawal symptoms. Yes, these wonderful pills work, but they can’t fix internal struggles and underlying causes of depression. I became addicted to Lamictal and Pristiq over the last 6 years. I craved the lessening of flight or fight mechanisms that caused me to feel constant anxiety and fear. I would do anything to get it, and then I hit an insurance doughnut hole. My pills shot up to 400.00 per month. Then I had to advocate for myself in extreme withdrawal (withdrawal isn’t just for illegal drug addicts) because my lack of healthcare and demographics left me without a psychiatrist. Without preventative healthcare and constant monitoring, these pills can became quickly toxic. I’ve suffered most of the side effects advertised by the manufacturer, and I’ve been hospitalized because of pancreatitis caused by Pristiq. I am pill free for over 9 months and there’s not much of a change in me. However, my chest is filled with adrenaline when I’m talking to others, and I’m in constant pain without pills or medication. Other than that I’m happy and I’m not depressed. I’m non-suicidal, I look forward to the newest films, play video games and if math isn’t involved, I’m a straight A student, I run, enjoy good food and music, I also love sunny days. I’m just sad because it’s hard to communicate with others. Most of the time my frustration boils over into non-violent rants or disagreeable conversations with others. This leads to rampant misunderstandings with people sicker than I am. I also have a global learning disability that is mistaken for a host of other issues, so things haven’t been easy. I’ve had to drop out of college because I can’t seem to grasp math (I have a BA in Fine Art) and I’m frustrated. I actually love life and I only wish to get well and surpass my limitations. My advice? Vote for public healthcare reform, whether we know it or not, the only way things will get better is with reform. Look at the voting records of each candidate and do not vote against your best interests. Keep your job for insurance reasons: Our fear of a public healthcare system gives us little back up. Our insurance for the mentally ill is poor, and the mentally ill are constantly being misunderstood and railroaded into plans that will not help them; if you have kids, think very hard about putting your kids on pills. I speak from experience and not psychosis. You don’t want to slap that sort of potentially life limiting stigma on a kid.
Paxil is the devels drug. if you have anxiety dont’t get on this drug unless you want to be on it for life! I have tried alot of them for severe anxiety from a brain injury i got in the military. which they dont do anything for you at all!!!!! They are taking me off diazepam which works great. but some scientist thinks it makes you worse. Well i have plenty of experience and they dont do what these doctors say. I think its all abunch of bullshit. These doctors are full of shit. I am so scared of them my skin crawl. why the FDA doesn’t get rid of the old bullshit antidepressants are just crazy.Like paxil its like i said the devels drug.you don’t have to believe me just read about some of the side effects from them. I personally can’t take any of them!!!!
I started taking citalopram fifteen years ago. Jung said that depression should be regarded teleologically, ie. that it was a symptom of internal struggle and I increasingly believe this. He also believed that man was inherently spiritual (he actually said ‘religious’ but perhaps that’s a little too provocative for today) and that Western society’s inexorable charge towards secularism was potentially catastrophic. Psychotherapy (and certainly not just CBT) remains for me, an essential way of recognising and liberating the repressions which have caused my mental ill health. I am though, also encouraged by research showing that components of the brain (the hypothalumus, hippocampus I think) have been shown to be diminished in size in the brain of the depressed person and that those components are restored to approaching their normal size with successful use of anti depressant medication and psychotherapy.
The ‘magic bullet,’ for ‘depression’ if ever it is devised, may be the thing which takes away our ‘angels’ aswell as our ‘demons.’ Can we have one without the other? Perhaps a society which offers only approbrium to our own sacred, internal givens is something we should hammer ourselves down to accept. We can repress everything so that we ‘fit.’ Or we can take medication which enables us to accept the unacceptable, numbs us to the unconsciousness of a world at which our spirits are internally screaming .
”It’s because of people like you that people like me have to take pills” is the slogan I once saw on a t-shirt. There is more than a grain of truth in that I believe.
If you have got this far, then thank you for reading. As ever, giving of myself is the strongest of therapy.
Here is a new story for any SSRI anthology.
I have been on fluoxetine for the better part of the past 25 years. I have never actually been diagnosed with depression but was put on it for a terrible bulimia that was threatening my future and my life. Within weeks, I was better and then stayed on at 20mg for 2 more years as I navigated the stresses of medical school. Then tried to wean myself off again. And again and again. Regardless of my life circumstances, coming off it inevitably has put me into depressions I had never experienced BEFORE ever taking this. Needless to say, I was profoundly depressed throughout 2 pregnancies and breastfeeding periods because I refused to take it, worrying that it would somehow affect my children.
Yesterday I saw a patient who started taking fluoxetine as a trial because he was convinced it would help with his amotivational state (despite not having a clear diagnosis of depression), only a “soft” diagnosis of depression. Now he tells me he cannot get off it because he gets more depressed and edgy than he ever was in the past, despite all sorts of life adversity. I want someone to convince me that SSRIs do not down-regulate receptors in some sort of permanent and damaging way. And I bet there is no one out there who can. Thanks for reading this. Lori
not sure if this will work. So not want to brief my story, and how serious it is to the brain, after 18 years on paxil, 20mg. the 30 for the last of these few months. Went downhill from there, and suicide attemtp not long ago
Whereas I had the opposite effect. I went on fluoxetine due to experiencing what I’d call mild depression. Worked very well – after going off them after 18 months, the same symptoms returned, and otherwise everything else feels fine.
Read Dr. Kelly Brogan’s new book A Mind of Your Own. I’ve been on SSRI’s for 20 years now. Numerous attempts to come off have failed 🙁 I am afraid I will be on them for life. I can’t go back in time, but if I could, I would have never gotten on them in the first place. I think my problems originally started from hormone and thyroid imbalances. I would go back and fix those first, but I can’t now. Hopefully Dr. Brogan’s book will save lots of other people though!
I have that book but I get upset every time I start to read it. I am stuck on ADs too. 18 years of them. Been on every cocktail of them. Very sad.
If psychiatrists were not around to prescribe all these antidepressants what function would they have? Isn’t it in their best interest to keep supplying their patients with narcotics?
I am currently weaning myself off of Effexor. While I have been on antidepressants for the last 12 years I have found they just don’t work anymore and I am not willing to keep trying other medications. I want to quit using them so perhaps my brain will start working properly again.
My wife is on effexor for over 20 years I feel their not working her mood swings are terrible hit me a few times even in front of our son told her doctor loads of times he just said to increase her medication my sin and I had a bad year in 2015 feel we have nowhere to turn her family dont want to know their leaving it up to me I work full time nights have to clean the house because my wife wont do it she minds her mother who is 90 she blames me and everybody for her life the way it turned out im doing my best cant put up with her mood swings any more want to leave with my son but he loves my wife very much and I know he will resent me for taking him away from her want to help and understand but she just take the medication her doctor is giving her
Hi Finbarr
A quite wise psychologist pointed out to my wife (when I was depressed) that her first job was to take care of herself or she couldn’t help take care of me.
In my opinion, depression is a family issue. It affects everyone and it is probably affecting your son as it affects you. I’m not saying your wife’s depression is harming him but it will be affecting his worldview.
Can you get some temporary separation? Being a caretaker burns people out and you and your son may need a respite break and it may be workable if your son sees it as a positive thing and yet not a permanent thing.
I was taking effexor clouds and amitriptyline together for over 25 years and after spending the last year stopping them. I am so shocked as to how they were not suitable for me. I can only see this now my body is clean from these meds. But over the years so many relapse,psychotic episode’s I now believe was the combination. I blamed everyone and everything for these episode’s, I had attempted suicide on a handful of occasions believing that was my only escape.I can honestly say I’ve never felt stronger mentally since stopping them and only wish I had the courage to have done it year’s ago. I feel I’ve wasted too much of life surviving rather than living. We are trusting doctors to treat us when in fact it’s all about pharmaceutical companies and nothing to do with our best interests. At 14 yrs old I believed that these meds would help me and I’d be suicidal without. At 42 ive woken up and realised that they’ve caused more damage mentally aswell as physically. If only I’d realised before!
Did you not have all kinds of withdrawals?How slowly did you taper?
Ive been on Various medication. For the past 12 years.
First remeron.
Then I was put on effexor for the past 10 years.
Every time I wanted to stop my psychiatrist said you probably need it. I had mild depression as I lost my youth love when I was 18. They all had me stop in a 2 week to 1 month timespam. I’ve said multiple times this was to fast. I had such severe withdrawal symptoms brainzaps hearing los in flashes. Unable to do anything productive for weeks. Heavy depression struck back at me worse then I ever experienced and every time was put back on the medication after a few months.
I’ve asked multiple times to withdraw very slow and in my opinion my brain was so used to the “captured” serotonin that if it is not there my brain doesn’t adjust and misfires causing the severe brainzaps and sudden exposure caused depression as wel. As my brain was not used / wired to not having antidepressants.
I stopped treatment and my doctor prescribed my effor. I lowered my dosage and when I felt good for at least a month I lowered dosage again. Every time let my brain and symptoms catch up to a state like I was on the medication. The lowest dose I opened capsules weight contents and rebuild the capsule. Lowering down in small amounts. As I knew I had most symptoms then.
As a alternative to the serotine medication. I bought 5htp. It has a warning not to take with ssri and snri’s because it increases serotonin in a natural way. I started taking these a week after I totally quit. The withdrawal symptoms almost vanished. Only with 50mg a day.
Now I can cry uncontrollably. Without feeling bad. I don’t feel depressed. And I can stop the 5htp without a issue but feel more depressed without it.
For the crying isn’t it supposed to be uncontrollably. It feels that a lot of things that happened over the past years I can now give some spot in my life. The crying got less over time.
Did I break this addictive cycle? I really don’t know. Doctors call it dependency. For me it felt like pure addiction.
I’m now doing thing in life because I feel and take action. I’ve been procrastinating for years on medication it couldn’t bother me anyway.
Good for you!!!!!i was on AD’s for 16 years THERES HOPE !! Amitripiline for 4 years and I’ve weined off pristiq it took 5 months of weining and now 3 months off completely and it took 4 months weining off Amitripiline and 4 months off that now so 8 months in total since starting wein. It was hard and still is hard. But I’m doing it. I wasn’t depressed I was put on for severe panic and anxiety. Of course I have that again but I will say its lessened threw the last few months. I will it go back on. It’s so hard to get off but please don’t give in. Wein EVER SO SLOWLY. LIKE I DID MORSEL BY MORSEL. There’s hope and I’ve got a wonderful husband who keeps telling me I’m strong and things will get better day by day week by week and they will. I believe and pray. And threw this whole thing after coming off I got stomach issues but I’m working on them now too. A up ride is I’ve lost the 27 pounds I gaining in the 16 year time. Please stay strong if I can do this ANYONE CAN.
I took Lexapro and later added Adderall for several years. I became addicted to the euphoric feeling short acting Adderall gives you when combined with coffee. I started drinking wine in the evening to come own more gently.
Eventually I weaned off the Lexapro and no noticed no difference. I did this when I was cut off severely in heavy, fast moving traffic on the highway. I managed to break and avoid what would have been a horrible multi car collision, but I felt nothing. No adrenaline, no concern, no heart racing, just meh. I realized that fight or flight feeling is there to save your life. I also realized I was probably missing a lot of other emotions that make life interesting as well.
Unfortunately, I stayed on the Adderall and that was a huge mistake. By that time I was at a high dose. Without Lexapro to balance it, I became OCD, paranoid, unpredictably angry, and had hallucinations (I think, God I hope they were hallucinations). I tore into my own skin, would let it heal, then do it again. It was so disturbing to my friends and family. I lost relationships, jobs. It hurt my son. I wouldn’t tell my doctor because I really thought I needed the Adderall by then.
I finally stopped for good in December and I am so happy to be sane again, but in the meantime I lost my self confidence, the respect of family, and my partner who just couldn’t take it anymore. I am depressed. now probably even more than when I started taking meds five years ago. I have considered returning to Lexapro because the depression is excruciating. But right now, I am holding off trying to find my way out of the rabbit hole by myself.
Jen your story really struck a chord.. All I can say is have faith you will get through it! I was never prescribed adderall but have struggled with using it for 3 years in college as well as other drugs to cope with stress over school and depression/anxiety… Eventually I had many of the same symptoms you were having with it and I was diagnosed with bipolar, schizoaffective, depression, psychotic, etc and put on so many meds I couldn’t even get out of bed without the adderall. Went off the antipsychotic/mood stabilizing meds and the adderall. Now haven’t used it for 3 months and I am so happy! My depression and mood swings are gone. I am on wellbutrin which helps me focus like adderall did without the high and is an antidepressant- plus it helped me quit smoking cigarettes! I am starting to create good habits to help me not go back to it when I return for my final year of college and I hope they work because I have relapsed before.. Adderall is a really dangerous drug!!
Hi- I read your post and I’ve been depressed since about 13 and been on every drug I think that is on the market and I currently in the past 6 months took myself off Effexor as I self medicate often as I believe my brain needs to relax for a bit. I’m currently taking my adderall and xanax only as needed, but I have never ever felt a high feeling or speed like on them like everyone says. I’m actually calling my dr. tom as I’m back in my depressed mode and I need to get back on something and that is how I came across this site I’m trying to research my own drug to take as I do often. I try to think I know what will work best for me as I think all this medication is so bad but idk what more I can do I’ve been depressed since I was 6 and nothing seems to change and I”m 40 now. I ask myself everyday will I ever be happy?
I’m slowly coming to terms with my father passing away two years ago, ever since I was young he was battling manic depression. I remember seeing the tablets he took for depression and the several for the side effects, and I can’t help think that all the drugs that he took didn’t help his situation. From me being of a young age I remember 20 years of him battling the horrific illness, and I wish they knew then what is known now. I’m sure drugs can help, but I don’t think they are the answer, especially for a prolonged period.
If i could go back 16 years and never take a antidepressants i would. I took effexor for 5 years which i cold turkeyed and had to go on prozac for the withdrawl nightmare. I stayed on prozac for 10 years at below theraputic dose (7-10Mg daily) in 2014 i stopped the prozac again cold turkey, the withdrawl did not hit for 2 months but i have been comppetley incapitated since, i ran the london marathon in 2013 but am unable to walk 50 yards, i have suicidal depression something i had never experienced previous to this. I will never take another AD, they have ruined my life.
It’s interesting that you say that antidepressants ruined your life when it sounds like you were better when you were on them. I have been off my zoloft for a few weeks now and I have gotten more and more depressed since then. I think that when I start to do better, I get under the assumption that “I got this” and that I can ween myself off of the meds. Every time I do, though, my life gets worse. Maybe it’s not the antidepressants that are the problem…
Exact same thing for me on zoloft also , everytime I start feeling good I tell myself I don’t need them anymore and can go on feeling good like this. But relapse everytime like a month or 2 after. Off of them atm for about 4 weeks and anxiety and depression coming back and everything is just going bad
Well seen as i have been diagnosed with drug induced neuropathy i’m pretty sure it is the drugs. Constant tinnitus,pain and chronic insomnia. Drugs are tested for 6 months after that you’re the guinea pig.
My 15 year old daughter began taking antidepressants a few years ago, but over the past year, she has been hospitalized 4 times for depression and suicidal thoughts. Thankfully, she has never made an actual attempt. She has been home for about a month now from her most recent hospitalization and is worse than ever, in terms of her depression. We have been tweaking her meds regularly, hoping to find the right mix. We have tried numerous anti depressants, mood stabilizers, anxiety meds, ADD meds, etc. No matter how much of anything she takes at night, she still wakes multiple times during the night. At one point, she was taking 4 Trazedone – still waking. Added one Serequel – same waking. Added a second Serequel – no change. At that point, we stopped all of taking either of those and we are on another combo at this point. She is becoming withdrawn, hates going to school, and doesn’t want to be around kids her age. She used to be the happiest, bubbliest girl you have ever known. I have been wondering if we should stop with all the meds and see if she can become herself again. I’m not sure what to do and I don’t want to make a mistake that could do more harm than good.
Does anyone have any experience taking their teenager off these meds?
Cindy, I would like to say I feel your pain, but I probably would be mistaken. As awful as it is to have depression yourself, I can only imagine it must be even harder to watch your child struggle with it.
I myself have had ADHD my entire life, but with treatment with Adderall, I was a happy and hardworking kid and teenager. Sometime between the ages of 18 and 19 I stopped feeling “right”.
It took me almost 2 years, and quite a bit of encouragement from my girlfriend to finally go see a counselor. After only one visit, it was clear that my suspicions were correct, I had depression. I have been on anti depressants ever since (I’m now 25).
But lately, it’s as if a switch has been flipped, and they no longer seem to work. I have a job I love, but now I can hardly bear not calling out or leaving early, and I’ve gone from being one of the best workers, to mediocre at best.
Anyways, I’m rambling now as usually happens when I get started on this topic. My main point I would like to make is that I would like to commend you for being so understanding and supportive as a parent. I myself am fortunate enough to have a father who deals with the same issues, as well as a host of other, more serious mental health problems. He has always been extremely supportive, and I can tell you from experience it really makes a world of difference.
Also I really wish there was something I was able to do to help you and your daughter. Depression has become the number once obstacle in my life and I have great sympathy for fellow sufferers and their loved ones.
If you ever need someone to talk to, please feel free to email me at Adamhoyt@live.com. The same goes for your daughter, maybe being able to talk to someone who understands what she is going through might possibly help. Either way, good luck and best wishes.
Hi, My 17 year old daughter was prescribed prozac off label for migrating pain related to fibromyalgia. In less than 2 months it turned nightmarish. She was hearing voices, seeing things, agitated, restless, bored, brooding, had impulses and compulsions that felt like they did not come from herself. She couldn’t think clear enough to do school work and felt emotionally detached. She was terrified. Previously she ran cross country, participated in speech and debate, studied piano at Vanderbilt for 6 years, and was very successful academically and socially. Following a taper off the prozac 5 months later, she is still experiencing horrible effects. I know this is not everyones reaction to prozac, but please watch your kiddo when they are on mind altering drugs. They can do damage.
To taper she took kavinace, dopa plus, magnesium, cod liver oil, vitamin d, and a metagenics multiple. She could not tolerate methylated b vitamins. They made her feel crazy. So she avoids them.
Hi Cindy. If I could do it all over again I would never had allowed my young son to take medication for his behavior problems. After years of prescription drugs, behavioral hospitals, and psychotherapy he has now become a recovering addict of drugs AND prescription drugs. What has worked the best for us is spirituality, exercise daily and got eating habits. Don’t ever give up. The battle isn’t over.
Dear Cindy, Please read Anatomy of an Epidemic by Robert Whittaker!
In my experience antidepressants don’t “fix” anything but gives one space to live. There may be other things going on – I couldn’t sleep well with fluoxetine, but it turned out to be a hormone medication I was taking instead.
I was a teen taking those meds. Take her off them, not only is Serequel dangerous, it’s only helped to shut me down. Serequel worked great for insomnia. Ask the doctor about Lamictal and Pristiq. See how she does on it. I am not a doctor, and I am not an advocate of these drugs for the long term, but they will give her some relief. Don’t let them put her on generics if she’s doing well. That will throw her into a serious withdrawal and derail her recovery. Make sure to have the doctor ween her off Pristiq and Lamictal after a while. I had to recover cold turkey and it wasn’t pretty. I had some serious side effects as a result of being on them for 6 years, so I had to quit them.
Here’s the last part, REMOVE HER FROM ALL. DANGEROUS PSYCH MEDS, talk to her, treat her well, think before you talk poorly about her, or stigmatize her as the black sheep of the family. Make sure you’re not paying someone to talk to her, you talk to her instead
,and encourage your family to follow your lead. Communication is key, listen to her feelings and practice compassion and patience. Also, have her get involved in meditation, mindfulness training, pets and excersize also help. Good luck on the ultimate journey, parenthood!
I spent twenty five years in difficulty with psychotropic medications only to find out I never needed them. I did not even have the liver enzyme , like 10% of all Caucasians, that cannot even metabolize most psychtropic drugs. Read my story Psych Trap by Antoinette Kirby RN available at Amazon or Balboa online books. I was able to get off all of them and get my life back. Healing can happen. Depression does not have to be a life sentence. We have no proof of any biological disease with it.
Toni, can you share how you got off the meds? What did you do and or take to help you recover?
I was prescribed Prozac upon returning from a time away from home that made me very depressed due to separation from my teenage son. I moved from that briefly to Buspar and then to Celexa. Dosage was always minimal. I also added gabapentin to help with sleep. The problem with anti-depressants is the complacency they can bring. People wind up taking them for longer than needed, if they were ever needed in the first place. They ought to be for acute and severe situations.
I didn’t really need antidepressants for my situation. That was an episodic depression brought on by events. They were prescribed by a family practice doctor, though likely anyone would have prescribed them as they were very popular in the late 90s. Family practice MDs ought not to be prescribing these drugs as they know almost nothing about them except what the drug companies tell them.
I discontinued Celexa almost five years ago, and discontinued a miniscule dose of gabapentin about six months ago. Even withdrawing from a tiny dose of gabapentin causes a reaction (panicky nightmares, etc. see other forums for various reactions). After going off Celexa I have lost about 30 pounds, back to my college weight. I walk daily and do Bikram Yoga several times a week. I also use supplements like magnesium and Kavinace for sleep.
However, I feel that I now have the chronic depression as described in the tardive dysphoria literature. It was worse in the first two years, which incidentally also coincided with a forced retirement and other disconnects. Normally I would have bounced back from a career setback like that, but I haven’t. No direction or follow-through and periodic week-long episodes of dysphoria and negativity. Alas these conditions work against finding new associations, keeping old friends and starting new projects. Constantly feeling that I am in the wrong place, wishing I had a different life than the one I do, recalling times when I did fun things and feeling powerless to change anything other than the routine stuff having to do with the body, exercise and diet.
I will never take an anti-depressant again. I would rather suffer through this with my brain doing its best than take the huge risk of tampering with it. But it can be discouraging. Activities and socializing help. The definitions and research are useful as they put a box around what is happening and point a direction for solutions. But I am still looking for recommendations on supplements to take or things to do, or some indication that eventually you get your old, only-occasionally-slightly-down brain back. The one that gets excited about things and follows through on projects.
For withdrawing, in case it hasn’t been mentioned, other forums describe a tapering method. You need to step down in intervals of at least two weeks, maybe more, with baby steps. Get a pill-splitter for tablets. If the lowest dose capsule costs too much due to being rarely prescribed, take the capsule apart. But I would prepare for a long process and do everything you can around the edges to make yourself healthy. Alas, few providers know anything about this recovery process. And of course they now all have a strong cognitive bias, not to mention a potential legal issue, with recognizing the harm these drugs can do.
Hi Eleanor,
How have you been feeling lately?
As far as additional helpful supplements are concerned, have you looked into 5-HTP and/or Tyrosine?
Also, Omegas, Vitamin D and B-complex are essential brain nourishing supplements/vitamins.
Another consideration is Ashwaganda (or Indian Ginseng) for energy and stress management.
Sending you smiles and good wishes 🙂
I was just going to suggest something similar. I have recently read a number of books about natural ways to restore your brain chemistry which seem to make perfect, logical sense.
In my opinion the best and most accessible is The Mood Cure by Julia Ross, which I would highly recommend, but there are quite a few others, one of which is available as a PDF download for free and is called The Way up from Down -it’ll come up if you google it.
Please check them out if you would like to learn more about how brain chemistry affects your mood -I have been amazed by what I have learnt! Good luck.
Thank you for writing this article. It reads very similar to my own life. I’ve tried to explain my thoughts on the damage anti-depressants have done to my brain, body, and life. Most people cannot understand. And, each Dr or therapist I see just push the next medication. I don’t know if the damage can be undone. I’m not thrilled to have started yet another med last week, one I had tried in the past and worked ok for a while, until it didn’t. I’m glad I found you online. I look forward to reading more.
I am now 47 years old and have been medicated with one medication after another for depression and bipolar depression and anxiety. This started at age 18. Over the years, my functioning deteriorated and I started having more frequent and more severe episodes of deep depression. The last combination I was on was adderall and cymbalta. I was so ill last year that I was referred for ECT. The neuropsych that I saw told me to come off of my medication first (slowly) and see how I feel. He said many people who have been on meds a long time start to feel worse over time and that they are finding out that these meds do a lot more than they thought. He told me straight out that they soon might not even be able to call them SSRI’s anymore. This is a very scary thought to me. I always knew they didn’t know exactly how they worked, but then how could they even guess?
Needless to say, I took a year and weaned myself off. I had to go very slow with even just 20 mg of Cymbalta, which was harder than the Adderall. It has been a month or so since I stopped taking my six tiny beads from the capsule. I am feeling much better, having added 3,000 mg. of Niacin (the flushing kind) to my healing regime. But I am still not ok. Over the years, I have experienced a sort of cognitive decline and loss of energy.
I know this is going to take time to heal my brain to the best it can be after all this, but I do feel much better now. I am sad for how depression and these meds and all their adverse affects about ruined my life. I hope I can feel normal some day, but I can feel my brain trying to rewire and heal and it is interesting.
Hi Cat,
Did you go through with the ECT? How are you feeling now?
I have been on SSRI’s since they first came out in the late 80’s. I was a bright, highly intuitive, creative graduate student but I struggled with horrendouse depression/anxiety. Naively I agreed to take these “benign” pills and thus began my slow decline into becoming a “happy idiot”. The cost to my personal and professional life has been beyond repair. I was a high-achieving, super-student in a very difficult architecture program and was a model to my family and friends before antidepressants…after years on the drugs I lost friends, family and most of my motivation to do anything about the downward slide of my life and found myself nearly homeless. Due to the spellbinding effect of these drugs it took a long time for me to figure out the med.s may be not only the cause of personal difficulties but also causing cognitve impairment and severe memory loss. I managed to eke out a career in my profession after graduate school (when I started on the drugs) but it was a constant struggle, far below what would’ve been expected of such a promising student. Finally after about 17 years on Prozac/Paxil I stumbled upon the discovery that when I reduced med.s my cognition and ability to perform my job was VASTLY improved. This began my experimentation with tapering and eventually discovering via internet that others were going through similar experiences. It’s been 7 years since I “woke up” and I have dropped from an excessively high dose to very minimal dose now. I have found through painful tapering that there seems to be an absolute minimum dose that I can reach and beyond that it’s scary; meaning my brain will not recover to my pre-medicated state even after 2 years of suffering/willing and waiting for healing. My point is: I have learned that long-term neurobiological/physiological damage IS a reality. My profession requires absolute full mental functioning, fast cognition and excellent memory- all of which have been stolen from me due to SSRI’s. On a final note; I have determined to “profit” (not financially certainly) from my losses and not be forever grieved about my losses but to make the best of what I have left…however I feel it is a moral imperative for me to speak my truth and to warn others of the nightmare ahead if one persists in long-term SSRI use. I advocate for the Truth to be disclosed to consumers/patients. INFORMED CONSENT…and allow the patient/doctor to weigh the risk/benefits. If one is struggling with depression one should learn as much as possible about the psyche through psychology, have maximum Love and support/empathy AND, what has turned out to be most helpful for me, seek spirituality; i.e. God/Universe/Source/Conciousness, whatever speaks to you. All the best to those seeking for a way out of depression and medicated stupor. There IS an answer but it takes a combination of hard work and determination and frankly, faith. CSC
Also look for underlying causes to the depression, it can be a symptom as well as its own disease. After second son was born and I got through the post partum depression/anxiety, I had surgery done to fix my heavy periods, (by psych standards anemic enough to cause depression but not enough to qualify for a blood transfusion so not much to be done other than the pill/surgery) and all the sudden I started needing less medication. I think there needs to be more attention to depression as a symptom of a bigger issue than oh let’s throw you on an antidepressant and ignore the underlying cause. I’m stuck right now where I’ve had many problems with the meds if they work I’m fine for awhile until the underlying problem is fixed then the meds fail to work anymore but not sure I’m ready to go off yet. Last drug I tried was great on my brain chemistry but horrid on my lungs so I’ll have to call later in the week and let them know for sure it’s the meds can I come in and discuss where we go from here. (not sure what else to do outside of another class of drugs) I’ve had those stupid drugs cause a major worsening of depression that I’m better off without the drug. The next problem gets to be I’ll just have to be super careful that I avoid situations that cause relapse (hanging out with worriers and not gracefully stepping away from them) For a smart organ the chemicals can be stupid
Hello Zoe, your story is interesting to me for some reasons. I find myself into very similar circumstances. I would like to make you a question- if possibile. is there a way to contact you?
I am becoming increasingly concerned with an aspect of Fava’s et al’s work and that is the term tardive dysphoria or antidepressant induced depression thanks to “oppositional tolerance” It seems the longer someone is on an antidepressant the more the brain tries to compensate and this turns off the brains natural ability to balance itself . Of even greater concern is those teenagers placed on SSRI’s for OCD, depression and anxiety that we may be relegating to a life long problem with chronic depression that is treatment resistant. I sure hope the paradigm shift with the use of Transcranial Magnetic Stimulation, the drug free approach can do for depression what other technologies are doing for other disorders. Things to Google are TMS and depression and Tardive Dysphoria.
I would not count on TMS as your magic bullet. In 2007, the TMS machine failed to get approval from the FDA due to clear lack of efficacy, i.e. it did not work better than placebo. Then the manufacturer “mined” the data from the failed study to see if there was some subgroup of subjects for which the treatment was better than placebo. They did find such a group, those patients that had failed to respond to exactly one antidepressant. Not zero, not more than one, only one. Now at this point, they should have recruited new subjects who had failed to respond to exactly one antidepressant, and run a new clinical trial with them. But instead, they re-submitted the data from the failed 2007 trial, but only with the one antidepressant failures included. This is a totally illegitimate statistical procedure, and the FDA should never have allowed it. Nevertheless they did, and TMS was approved for those people who had failed to respond to exactly one antidepressant. Once approved for anything, TMS could be prescribed for anyone with depression, as long as the manufacturer was not officially promoting it for such off-label use. TMS clinics have sprouted up all over the country (put TMS into YouTube) making all sorts of ridiculous claims, not mentioning the
FDA’s very narrow indication for its use, which, as previously stated, was obtained by accepting a bogus statistical procedure. Most insurance will not cover it due to lack of demonstrated efficacy.
However, there are numerous anecdotes from patients all over the internet testifying to the miraculous recovery it brought to them. Lets see why this is largely placebo. The protocol for TMS is as follows: 4-5 treatment per week (each lasting 45 minutes or so) for 4-5 weeks, at about $500 per treatment. Now, a depressed patient who who starts getting out of the house and gets into a routine for such a period of time may well improve simply because of that, it is impossible to untangle that effect from the machine effect. In the 2007 study, there was a placebo group getting “sham” TMS to compare to the group getting “real” TMS, and except for the narrow group mentioned (exactly one antidepressant failure) there was no statistically different result from sham and real TMS groups.
This entire procedure in my opinion is based on marketing hype and placebo effect. Send patients to see a good CBT 4-5 times a week for 4-5 weeks, and the vast majority will improve, at $100-$150 per session instead of $500. In fact, many improve going only the standard once per week. Case closed.
Hi there,
I found this site via my husband. He and I are having very difficult times and one of the things that has come up in our counseling, as well as on-going talking, is my depression. We can almost map some really bad spells in our marriage with my deep depressions. I don’t know why we never noticed this until now….
In any case, I have been an on-again, off-again meds woman. My last meds were prescribed (2011) to treat my all of a sudden panic/anxiety that traced with my menstrual cycle. I was diagnosed with PMDD and my doctor had me taking Proxac for the duration of my PMS, only to then stop once my period hit. I have always had really bad menstrual cycles, but this was the worst ever. (I’m 39)
When I noticed the Proxac was making me feel pretty good, in general, we decided I should take it full-time. About 8 months after the full-time, it stopped working. But my PMDD was a mess and my actual cycle was not regulated, so my doctor put me on the Pill (Sprintec) and said after my cycle regulated, we would check about my depression. Basically get one going, then let’s check on the next.
My question is are there any women out there who deal with their depression and PMDD? The Sprintec has been a godsend and my cycle is regulated and not nearly as severe, but my depression still needs attention. I have an appointment with my doctor this week and I am nervous about being medicated again, but I am also nervous about NOT being medicated again.
My marriage is a shambles and my husband and I are seeing a therapist, so while we have some acute issues to deal with that explain the immediate, I am still concerned with slipping into a deep depression while going through this process.
1. Sprintec has helped me, but I don’t have PMDD. But the main reason I switched to it (from Tri-Sprintec) is that I did notice my depression getting worse right before my period, so my ob/gyn suggested Sprintec. It did take awhile to make a difference though. How long have you been taking it?
2. If you’re not already, definitely go see a therapist separate from your husband. Continue the counseling with him, but also make sure you’re getting your own treatment and support. Individual therapy could help you handle the issues in your marriage, and also address your depression separate and apart from the marriage issues. Also, there are therapists who are more experienced with PMDD than others, so you could try to find one who seems well versed in PMDD, if that’s possible in the area that you live in and within the limits of your insurance or ability to pay out of pocket.
3. Is your doctor a psychiatrist? If not, please consider going to a psychiatrist for your medication and diagnosis. Maybe I’m biased, but I’ve never had a good experience with an internist / general practitioner when it comes to mental health issues, and if you have deep depressions, I think that warrants a visit to a specialist. Some psychiatrists also do a combination of therapy and meds, so you would only need to go to one doctor to get both, but sometimes they can be hard to find, especially if you’re not in a large city, and in my experience they generally do not take insurance. I truly believe it’s worth the cost, though, and many insurance plans reimburse for out of network visits after you meet a deductible and coinsurance amount.
4. If you’ve only tried Prozac, or only a limited number of meds and haven’t stayed on them for very long, I wouldn’t think of this in terms of meds vs. no meds just yet. Also, meds alone aren’t generally very effective, especially for depression or anxiety; they should be used in combination with therapy.
5. Prozac and all SSRIs take something like 6-8 weeks to work, when taken regularly. If you were initially told to only take it one week or 2 weeks per the month, and told that it would work instantly to treat the PMS, I don’t think this is sound advice. I’m pretty sure it’s not a drug that has an immediate effect in the way that other drugs do (e.g., antipsychotics).
6. There are also some good mood stabilizers out there that might help you. Something to ask about, at least. I’m not sure if some are PMDD-specific, but if you’re having trouble with mood regulation, this is something to consider. Lamictal is one of the mood stabilizers, and it has helped me recently. It also doesn’t have much in the way of side effects, with the exception of a very rare condition called Stevens-Johnson syndrome, but if you start at a low dose and then increase it slowly, that’s supposed to lower the risk of that syndrome as well as any other potential side effects.
I’m not an expert in all of this, nor am I trying to answer for John. These are just my opinions, but I hope they’re somewhat helpful.
Jenny,
Thank you so much for your response. I have had a very good relationship with my GP and she has referred me, when needed. She and I have an appt on Friday and I suspect that, if need be, she will refer me. I do not have insurance, though, so that may determine what course of action I may need to take.
I took Prozac for almost a year and when it did finally kick in (about 2 months?), it worked for a spell, but then didn’t. Neither me nor my doctor was expecting it to work ‘immediately’.
I may well start individual therapy, but at the moment, the couples therapy is all we can afford and it has been very helpful.
I will ask my doc about the mood stabilizers you suspected. I am not bipolar, but it may be that they could help. I am not really sure.
I do know I have gotten into a pretty deep depression and need some help. I have been very happy with my Sprintec (over a year of taking it) and whatever I will take, in addition, can’t interfere with it.
i have been on medication for 4 years can your medication stop working after four years
John, did you eventually withdraw from the Emsam and Lamictal, or are you still on them?
I haven’t worked my way through all your posts yet, but if you are still considering other medication alternatives, the older MAOIs might be a good option for you, since you responded to the Emsam. There are several older ones to choose from, and the dietary restrictions don’t really have be followed as strictly as some people think, the hypertension risk is not as great as it was first thought to be.
I’m on Parnate and just added Lamictal, but the Lamictal isn’t at a high enough dose yet to determine whether it’s helping. The Parnate works, but alone it isn’t enough, and I experience other (non-diet related) side effects at higher doses of it.
Curious to know whether your Emsam + Lamictal worked for you, and if not why not, what happened.
Thanks.
Hi, Jenny –
I phased out Emsam last year and am almost off Lamictal now. They had stopped making any difference, as far as I could tell, and I wanted to see how things went without any medications. I’m not averse to trying something else if I need to, but I am doing fine now. There are a couple of later posts describing how I tapered off – Lamictal (lamotrigine) has taken me much longer to withdraw from since it gave me some problems when I lowered the dose too quickly. I’m down to 25 mg now from 300 and expect to be off completely by next month. So I’ll see what happens. I’m glad you’ve found something that works. I tried 20 or so meds over as many years and had very limited success.
Thanks for the comment – do keep us posted on your progress.
John
Hi John,
Thanks for your reply. That’s what happened to me with the Parnate the first time around, it just stopped working after a few months. Seems like that happens to a lot of people with all of these antidepressants, they just stop working after awhile.
I’ve also gone through 20+ meds (I quickly lost count), from every category, plus tried other stuff off-label (e.g. stimulants), and finally tried ECT a couple months ago, and along the way have tried different types of therapies, and went inpatient several times… And after going through all this, it seemed like the only thing that made even a slight difference was Parnate. Which makes sense, since MAOIs are supposed to be the most effective drug for atypical depression. ECT did nothing, except mess with my memory. So I’m back on Parnate, but even with it, I still have periods of major downward mood swings, so it’s not a magic bullet, maybe none of these drugs are. I’m thinking now that the only way to get out of this (at least for me) is a combination of drugs + more years of intense therapy + new job or career + family support + lifestyle changes and self-help… It’s exhausting just contemplating all of this.
Sorry to hear that the Emsam and Lamictal didn’t work for you, but doing it meds-free may be the way to go, and on the plus side, you don’t have to worry about any side effects!
Jenny
For anybody taking antidepressants, this is a must-read article: http://www.madinamerica.com/2012/09/things-your-doctor-should-tell-you-about-antidepressants/
I took antidepressants every day for 26 years and then, when I was dying from them, I stopped (in 2001). Now I have terminally bad diabetes (glucose 450) but cannot tolerate insulin because it makes me suicidal. In fact, I cannot take any long-term medication for any physical illness because they all cause unbearable psychiatric symptoms. Nobody knows why but an immunologist and a psychiatrist with a Ph.D. in pharmacology are currently working on the problem.
You cannot imagine what long term damage you are doing to yourself by taking long term antidepressants.
In fact, the cure for depression is not drugs; it is action. The trigger for depression is the perception of powerlessness. The cure, therefore, is to reverse the trigger. Change your life, not your brain. For much more on this, see my blog http://behindthelockeddoors.wordpress.com/2013/03/29/the-enduring-damage-part-i/
That would be another reason the drugs would be counter-productive. Believing that you are incurably ill and cannot control your own behaviors only increases perception of powerlessness.
Hi John,
Thank you for your replies. In addition to terminating the Zoloft in November, 2011 (after 9 months of tapering), she started tapering off Lamictal in December (150mg). Now, 8 months later, she’s at 50 mg of Lamictal, and has been holding at that level for several months.
While she was tapering off the Zoloft, she was doing pretty well until she hit 25 mg. She started to feel uneasy in October at that level, and has been feeling uneasy since then. Because she felt she couldn’t feel any worse, she started the slow taper off lamotrigine in December 2011.
We’re not sure if the chest pressure, heart pounding, and generalized anxiety are coming from the elimination of Zoloft, or if it’s the withdrawal from lamotrigine. It’s the physiological symptoms that are so troubling.
She’s slowly developing a mindfulness practice, but she feels hijacked by her body. It doesn’t seem like her physical symptoms are related to a deficiency of serotonin and her symptoms don’t match up with what’s published about lamotrigine withdrawal.
What symptoms / effects are you feeling from tapering off lamotrigine? At what rate are you reducing dosage?
She’s had cardiac tests, and they show nothing wrong with the heart. So we’re assuming the physical symptoms are related to anxiety, and we’re hoping the mindfulness practices will help. She’s just so tired of feeling horrible day after day (it doesn’t help that she hates the field of work that she feels locked into for financial “security”).
Aryn
Hi, Aryn –
I think the specific reactions to any medication are going to vary with each person, especially when multiple meds are involved. Has she been tapering off under a psychiatrist’s supervision? As you may gather, I’m skeptical of doctor’s with a meds-and-more-meds approach, but the symptoms you describe sound something like panic attacks. Stress from staying in a line of work she hates can play a huge role in undermining health at multiple levels. Together with depression and anxiety, there are strong correlations between ongoing stress and heart rate variability, blood pressure, immune system, diabetes and other problems. Could she arrange for a leave of absence to see what difference removing the major source of stress would make? In any case, if she’s having this level of difficulty with withdrawal, I think a psychiatrist’s supervision is important, provided you have one you have confidence in.
John
Hi John,
Have you read anything that mentions how long it takes to restore neurobiological stability after withdrawing from SSRIs? Can the body recover from 30 years of antidepressant use? My partner took 9 months to withdraw from 175 mg of Zoloft and Risperdal (mg?). Now, 10 months later is overwhelmed with chest pressure, heart pounding, generalized anxiety, disrupted sleep, lack of enthusiasm… The symptoms have seemed to increase over the last 10 months. We have a great diet, take all the recommended supplements including amino acids, and exercise.
Thank you for any information you may have,
Aryn
How is your partner now? Did he/she go back on drugs?
30 years? Holly cow! Check out paxilprogress.org from some help. I think we can recover, but it take time, and a LOT of it! I am now 10 months off and still struggling although I have seen some improvements.
Hi, Aryn –
From what I’ve been able to learn, there is little research on the problem of withdrawal from long-term antidepressant use. (By long-term, I mean 10 years or more – not the 1 or 2 years of most studies.) Psychiatrists have become so convinced that many people need to stay on these drugs indefinitely but have no evidence about the long-term effects of dependence on these medications. I’ve been dealing with withdrawal from lamotrigine for six months but expect I will need to continue tapering off for a lot longer. The conventional advice for your partner would likely be to go back on the drugs, but psychiatrists like Nassir Ghaemi have questioned the logic of that conclusion. I wish there were an answer for you, but I believe we’re all in the dark on this crucial question.
John
I was on various antidepressants for almost 8 years and have recently come off using some IV nutrients and cranial electrical therapy. I also did some neurofeedback for a month and that helped level me out. Even with those things, and additional supplements, the withdrawal was very painful and I am currently still experiencing problems with depression and anxiety. Its important to note that my depression was never this bad prior to antidepressants. I had pretty bad anxiety which would make me depressed and upset sometimes, but never like now. Currently, most days of the week consist of low mood, fatigue, inability to concentrate, etc. Anxiety is not too bad, though.
I often wonder if my problems were made worse by long term antidepressant use and why the medical community does not try less powerful “medicines” first and only use the drugs as a last result? Perhaps many of us would not be stuck on antidepressants or other pysch drugs forever. I read that up to 95% of people who attempt to get off their psych drugs fail and go back on them. What is really going on here? Why are these “medicines” not lowering the rate of mental illness?
Hopefully I can pull through this. I told myself one year; one year being off psych drugs and see what happens. I may need to go back on, but the side effects are very severe for me and I literally would sleep 14 hours a day.
Hi, John –
I’m sorry to hear that you’ve had such a rough time with antidepressants. As you can see from these posts, I’ve wondered just as you have if depression weren’t worsened by the long term effect of the drugs. Although I never had severe side effects, the illness did become much more sustained, almost constant on the meds. Before that period – and I’ve been on these drugs for almost 20 years now – depression alternated regularly with periods when I was fine as a person and super-productive at work. I don’t know what’s wrong with psychiatry these days either. Treatment is so mechanical for most people – here’s a prescription after a 15 minute session. When you read about treatment by psychiatrists or look at the APA treatment guidelines for depression, they describe a wonderfully careful process that begins with a thorough assessment and therapy, and only then moves to meds if necessary. That sort of treatment, however, is probably only available to wealthier patients who don’t rely on insurance or community clinics.
I hope you have a good year off meds. I’m not surprised that people often get depressed after going off long-term use. The brain has come to rely on the action of these drugs and must take a while to restore neurobiological stability.
John
I have been reading Whitaker’s “Anatomy of an Epidemic” for a couple of weeks. I felt a little sick after going over the evidence he presents supporting “natural recovery” as opposed to the use of antidepressants. My longterm goal is to slowly withdraw from all my psychiatric meds. I expect to have some rebound depression, possibly rebound psychosis and mania. But I seem to keep having these from time to time anyway. My problem is not, however, the fear of relapse, but the fear of how my daily life is being impacted right now by the meds. I feel far too fatigued, disconnected, anxious, restless…all more or less constantly. With some of the meds I have tried, these side effects were severely disabling and kept me from fully engaging in life. Not so much now, but still too much to feel comfortable with. I feel I will never have a rich emotional life or steady and meaningful relationships or even the energy to do what I please on any given day while I am still taking 3 antidepressants, an antipsychotic and an anti-anxiety med. Yes, they may suppress the worrisome symptoms, but they also suppress my personality and zest for living.
Hi, Donna –
That’s a lot of drugs. From what I’m reading, prescribing several antidepressants isn’t well supported by the recent data, but I’ve had multiples in the past too. I”m sorry they don’t seem to be doing much for you. “Suppress my personality and zest for living” – that’s what I felt on various antidepressants. I wrote about this “side” effect on Storied Mind (Feeling Fine on Prozac) quite a while ago. The main effect was a feeling of detachment from everyone and an almost emotion-proof life. That’s a poor trade-off for getting away from despair and deep hopeless moods. Deadened feeling also happens to be the other defining symptom of depression in DSM. To meet the diagnostic criteria, you must have either depressed mood or anhedonia. So, what sort of help is that?
John
Hi, John. I’ve read about the theory of tardive dysphoria before and it certainly has me wondering, too. I haven’t had a really bad depressive bout for about 18 months and after hearing about the possibility of long-term antidepressant use possibly keeping us depressed, I’m considering – slowly – going off my Wellbutrin, which I’ve taken for probably more than 20 years. I’ve been doing a lot of EMDR and thinking that eventually, maybe I’ll have changed some of my brain patterns enough to not need the meds. I don’t know. I’m sure most of us are reluctant to take the chance of falling back down into that hole if we can help it, but on the other hand, if we have a good support system, the way back out may not be as horrible or as prolonged as we might imagine. I know I don’t ever want to again be in that place where I couldn’t be there for my family and then felt worse when my spouse would get angry with me for being depressed. Well, we’ve both learned some things since then but it is a horrible feeling when you believe you are making everyone around you angry and miserable.
I’m going to check out your reading suggestions so I can have an intelligent conversation with my psychiatrist the next time I see him. Thanks!
Hi, Judy –
I know how that fear works. The main reason I stayed on antidepressants that didn’t work for so long was fear that if I went off them I’d feel far worse. I need to find the studies on depression following withdrawal from drugs – it does happen, but as I say in the post that doesn’t surprise me. Sleeping pills have the effect of creating dependence on them for sleep. Naturally, if you stop taking them you’ll have insomnia again, but the question is how long would that last? How long would it take your body to get back to the internal balance it tries to achieve? I never tried to find out what would happen if I stopped antidepressants. I’m still nervous about stopping. No easy answers, more trial and error, I guess.
John
I am currently thinking of tapering off my meds and I can tell you it frightens me every day, I am 30 years old and have been on and off meds since I was 15. Whenever I went to the Doctor about feeling depressed again, the recommendation was always to find another cocktail of drugs that would work “better.” When I was 15, Prozac changed my life. I was shy and had mild depression, suddenly I was a new person, happy and talkative. I would go off my meds, “cured” as they say, only to be back on them in about 3 to 6 months. This created a fear in me to never stop taking them. Ive been on Prozac, then paxil (made me fat), then celexa, then all of those in combination with wellbutrin (which never seemed to help) and finally, lexapro. When I expressed concerns that I was afraid these drugs would stop working, the response has always been, don’t worry, there are so many drugs out there you could try. Endlessly medicated, as they say. My depression runs in my family, so it was easy to sell to me the idea that I needed this. Taking drugs always seemed to be preferable to being like my miserable relatives who never did. But if there is a genetic component to my illness, these drugs all worked..initially. But no one ever thought of the long term consequences..should I have only used them at rock bottom? Not at all? Should I continue to take them the rest of my life? I don’t trust western medicine to be able to help me, as it is driven by finding the next drug to cure you. I don’t know what I hate more, doctors prescribing me endless drugs to fix me, with no luck..or the person who tells me all i need is to improve diet and exercise and take vitamins. No one seems to understand what I really need. And neither do I.
Hi Colleen,
I understand your concerns, I’ve been there too, and I’ve asked myself (and doctors) the same questions before (and still do from time to time). It’s frustrating, this is a hard disease to treat, and it takes a lot of time and trial & error. But honestly I think you should try to find a doctor you can trust (a psychiatrist, not a primary care doctor, if possible), one that you can openly discuss your concerns with, and who will listen to you and take your concerns into account and discuss this with you until you both come to an agreement on an approach. Though if you’re really opposed to Western medicine right now, maybe focus on finding a good therapist instead, and discuss these same concerns with them. Finding someone you trust who will listen to you and try to find solutions for you is crucial. It may take some time (and money) to go and “interview” different psychiatrist and therapists, and I know not everyone has access to the same level of medical care, which is sad, but if you do, then it’s worth the time to find someone you like and trust.
Have you tried different types of therapy, and has any of it helped? I think many people would benefit the most from a combination of therapy and medicine, along with the other things you said, diet and exercise and vitamins and anything else that you discover that works for you. But I would urge you not to rule out Western medicine entirely, especially since it sounds like you have responded to drugs in the past, just maybe not the right ones for you, because the right one will be one that doesn’t stop working after awhile.
***I would worry far less about the long-term effects of these drugs than the short-term effects of not getting better.*** It’s true that they don’t know the long-term effects of these drugs, but there’s a lot of things that we don’t know the long-term effects of, and I believe that this is something that researchers are trying to study and hopefully we will know more eventually. But if you feel bad now, it needs to be addressed now, see if you can start trying various things to see what helps, or just one thing at a time, but don’t give up. Maybe you will need to be on a medication forever, but maybe you won’t, it’s just not possible to predict the future for everyone. Depression can’t be cured, but it can be managed, and that management may need to be drugs, but it can also be through learning new ways to cope.
Good luck to you.
Jenny
P.S. It sounds like you’ve mainly just tried one class of drugs, the SSRIs, with the exception of Wellbutrin. SSRIs didn’t help me either, but there are other categories out there, and some people need a combination of drugs.
Hi,
I do have a therapist and I have had numerous psychologist and therapists. To be honest, I have never gotten much out of it because I do not feel good after talking to a stranger. Just going stresses me out, and I try to keep going. Some I didn’t like, my current one I like..i just don’t enjoy sitting and talking. I have difficulty calming my mind enough to meditate as well. Ive tried writing in journals. Ive had these feelings since as long as i can remember, I just didn’t have a name for it back when i was small. I believe I am dysthymic and have always had small amounts of anxiety. Its hard to see how “talking” about something that is part of my biology will help me. Im trying cognitive therapy, but i don’t think my depression is due to life experiences or ways of thinking, it just IS. I think it could help me in times of major depressive disorder, which i am currently suffering from (bad breakup, left job due to bad boss, lost a pet) Ive often resigned myself to a lifetime of pills..each time I go off I’ve usually lasted about 3 months (which is about how long prozac persists I’m told). I recently ran out and couldn’t handle the withdrawal from them, i spend whole afternoons in bed. I don’t recommend cold turkey at all, I just ran out of $ for my prescription and lost my backup stash.
I can say that my pills make me gain weight and also fairly numb me. Sure, Im not crying anymore but my zest is gone..i often feel sedated and hungry constantly. So I hate taking them, but feeling depressed? Even worse. But, over time it seems to lose its effectiveness..so maybe these pills are great for short term depressive disorders..but not long term. And how many times can you switch to another pill..got to run out eventually, right? And they don’t even know how these pills really work. Makes me feel like a guinea pig..20 years later find out they made things worse..who knows?
Hi John,
I found your site while searching for wisdom about tapering off my daily 150mg of buproprion XL. I have been taking antidepressants for perhaps 30 years, and I am finally convinced that they do not cure anything but merely mask my mild depression. Worse, they have no doubt subtly changed my personality, by incorporating a sort of “always defeated” attitude into every day. In the last 3 months I have decided to wean off the buproprion because I feel so distinctly better physically (and mentally) as a result of going on a totally vegan diet. I exercise faithfully (walking and swimming), and the vegan diet gives me new energy and hence hope that I can forge ahead with the withdrawal symptoms.
So far so good. After 3-4 weeks I have cut down from 150mg/day to 75/day. I certainly feel the old “what’s the use?” feelings, plus increased irritability, as well as reclusiveness; but with the new sense of empowerment from my PLANTS ONLY diet I think I will be able to follow through with withdrawing buproprion from my system.
The real question or problem, as you are keenly aware, is what to do when I reach the detoxified stage, the point where I am off medication and have to rediscover and redefine what it means for me to feel “not depressed.” I sincerely believe that “normal” has been changed as a result of decades of addiction to antidepressants. I want to re-learn who I am, what my normal day-to-day emotions sans drug are, and thence live my life fully using the array of coping wisdom I have amassed over the years. I want to be back in touch with Who I Really Am rather than that guy who was always neutralized by antidepressants. Life has its natural ups and downs, and I am confident I can negotiate these variations “on my own power” rather than with the numbing of an antidepressant drug. Diet and exercise and meditation help, but the great and beautiful challenge of living is to face reality bravely with all the resources of my own personal character. It is not a question of “toughing it out without antidepressants,” but rather of rediscovering the immense power of my own inner resources (which have been muffled or deadened by those pills).
So to return to the present moment–I am forging ahead on 75mg of buproprion for the past 2 weeks or so. I think I shall try to stay at this level for at least a month. Then I might feel ready to cut that 75mg-tablet in half and take that half once per day for another month. Weaning is definitely the way to go, not cold turkey.
I have never suffered from what I would call severe clinical depression. The worst I have ever had would still be labeled mild depression. So I guess I’m lucky. However, why have various psychiatrists put me on such addictive drugs for this transitory, mild condition? Never should have happened.
Sometimes we need to change our lives, not merely adjust to them by taking a pill.
Thank you and best wishes.
I believe my partner is alive because of anti-depressants, so I think they are very valuable. She does want to get off them when she has worked through her feelings and is stable.
Long-term is an open question for her. The side effects (which there are bound to be) will need to be weighed up.
I’m wondering if there are differences with people who have an abused childhood – as she does; for these people it can mean creating a sense of ‘normal’ as the ‘normal’ was horrific. I don’t know of any research on this, if you do I’d love to know about it.
Hi, Evan –
There are so many stories like your partner’s. Lives of severely depressed and often suicidal patients have been saved, while others have had experiences like mine, sometimes with damaging side effects. That’s what makes the debate about antidepressants so passionate. It’s often put in absolute terms, as if the drugs were great or evil and nothing in between. Part of the problem is that most studies in the past didn’t separate effects on the mildly depressed from those with severe conditions. Recent studies are showing that mild to moderately depressed people get the least benefit and severely depressed the most from antidepressants.
The concerns I have come from my experience but also from the different ways people respond to the meds. No one knows why, but fortunately research is turning more and more to this question.
People will stay with whatever works for them. I think the only approach has to be pragmatic – the best treatment is whatever helps you.
John
I believe anti depressants may be valuable to those who are depressed. But my husband was put on them 7 years ago after one small panic attack and has become addicted to medication he doesnt really need. Shortly after starting meds his personality changed from a kind caring normal man into a monster. The things he has done on medication is quite digusting yet he thinks he has done no wrong. All our friends and family cant believe how much he has changed and how little he cares. We had a grandaughter born ten weeks ago and he hasnt even seen her or asked anything about her. Also our grandson who is 4 spent every weekend with us since he was 6 weeks old and now he doesnt care about him or even ask about him. He acts like he hates me for no reason other than that I have told him lying and gambling big money on credit cards is wrong and his behavior is out of character and has been for years. He had nothing when we met and I shared everything I had with him and now he has a well paid job he says everything is his. Needless to say our marriage is over as now he says I am crazy and he cant live with me anymore. He is happy looking for a new house to live in and I will have to live in a caravan park. After the house is sold and all the debt is paid back which is huge because of gambling debts and car after car added on to the mortgage ( he is never happy with his car and keeps changing them even though I beg him to stop) I may have enough to get a small park home. I am 53 with no way of getting a loan. He is younger than me with a good job and can get a loan. When we met I had a four bedroom two bathroom home and now I will be lucky to have somewhere to live. He doesnt care at all. This is the same man who adored me prior to starting medication and now I am nothing. Everyone can see that he changed but him. He is like a zombie when it comes to emotion but pretends to care when someone at his work is upset. He has put me through hell and I wish that doctor never prescribed those pills. The man I loved is long gone.